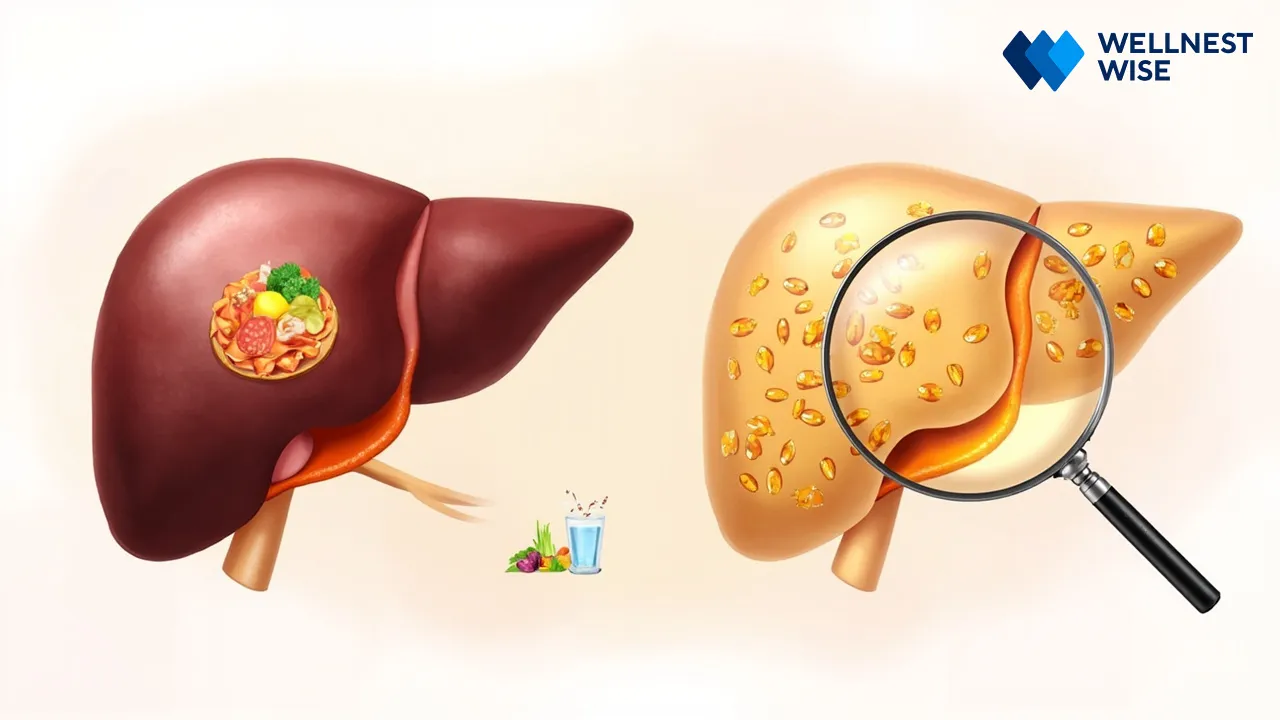
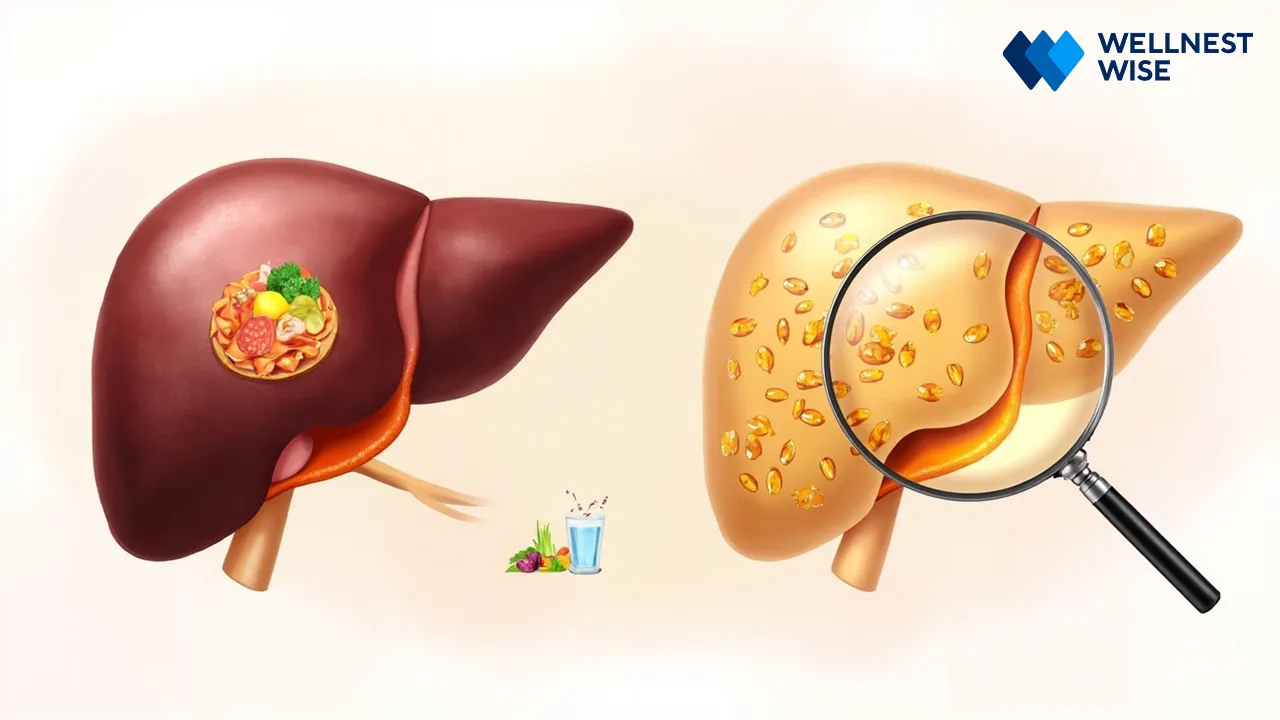
Imagine being told your liver, that incredible organ responsible for hundreds of vital functions, is struggling, silently accumulating fat. This is the reality for millions globally, and often, the first step towards feeling better isn’t a prescription, but a fork. Non-alcoholic fatty liver disease (NAFLD), a prevalent condition, is deeply intertwined with our diet, and making informed food choices can be a powerful catalyst for healing. This guide will help you navigate the dietary landscape, empowering you to nourish your liver back to health.
Understanding Non-Alcoholic Fatty Liver Disease (NAFLD) and Its Dietary Connection
It’s often a silent condition, developing without obvious symptoms, yet NAFLD has become a significant public health concern. Many discover they have it during routine check-ups or when investigating other health issues. Understanding what causes it and how deeply intertwined it is with our daily food choices is the crucial first step toward taking control.
What is NAFLD (Hepatic Steatosis) and Why Does Diet Matter?
Non-alcoholic fatty liver disease (NAFLD), also known as hepatic steatosis, is a condition where excessive fat builds up in the liver cells, not caused by heavy alcohol use. While it might sound benign, this fat accumulation can lead to inflammation and liver damage over time, potentially progressing to more severe conditions like non-alcoholic steatohepatitis (NASH), fibrosis, cirrhosis, and even liver cancer. What we eat directly influences how much fat accumulates in the liver. A diet rich in processed foods, unhealthy fats, and sugars forces the liver to work overtime, storing excess energy as fat. Conversely, a mindful diet can reduce this burden and promote liver health.
The Role of Diet in NAFLD Progression and Potential Reversal
Diet isn’t just a contributing factor to NAFLD; it’s often the primary driver and the most effective tool for its management and potential reversal. Research consistently shows that dietary changes, particularly those leading to modest weight loss (even 5-10% of body weight), can significantly reduce liver fat, improve liver enzymes, and decrease inflammation. This isn’t about extreme restriction but about making sustainable choices that support your liver’s natural functions.
“Many patients come to us feeling helpless after a NAFLD diagnosis,” shares a registered dietitian specializing in liver health. “But when they embrace simple dietary shifts – swapping sugary drinks for water, choosing whole grains over refined ones – we often see remarkable improvements in their liver function tests and overall well-being. It’s truly empowering.”
Recognizing the Metabolic Linkages: Insulin Resistance and Liver Health
A key player in the development and progression of NAFLD is insulin resistance. This occurs when your body’s cells don’t respond effectively to insulin, the hormone that helps regulate blood sugar. To compensate, your pancreas produces more insulin, leading to high levels in the blood. High insulin levels promote fat storage, especially in the liver, and can also trigger inflammation. Diets high in refined carbohydrates and sugars are major contributors to insulin resistance. By focusing on whole, unprocessed foods and managing blood sugar, you can directly address this metabolic imbalance and protect your liver. This interplay is a cornerstone of metabolic syndrome, a cluster of conditions often seen alongside NAFLD.
Essential Foods to Embrace for a Healthier Liver
Shifting to a liver-healthy diet isn’t about deprivation; it’s about celebrating a wealth of delicious, nutrient-dense foods that actively support your liver’s healing journey. Think of your plate as a canvas, ready to be filled with vibrant colors and wholesome ingredients that work in harmony with your body.
Fiber-Rich Whole Grains: Fueling Gut and Liver Health
Fiber is a superhero for your liver. Found abundantly in whole grains like oats, brown rice, quinoa, barley, and whole-wheat bread, fiber helps regulate blood sugar, promotes satiety, and supports a healthy gut microbiome. A thriving gut environment, in turn, reduces inflammation throughout the body, including the liver. When you choose whole grains, you’re not just getting fiber; you’re also benefiting from essential vitamins, minerals, and antioxidants that protect liver cells. Start your day with a bowl of oatmeal instead of sugary cereal, or swap white rice for quinoa at dinner.
Lean Proteins: Supporting Liver Repair and Function
Adequate lean protein intake is vital for liver health. Proteins provide the essential amino acids necessary for liver repair, regeneration, and the production of enzymes involved in detoxification. They also help you feel full, which can aid in weight management – a critical aspect of NAFLD improvement.
- Skinless chicken breast and turkey: Excellent sources of lean protein, versatile for many dishes.
- Various fish like salmon, cod, and tuna: Beyond protein, many fish, especially fatty fish like salmon, provide beneficial omega-3 fatty acids.
- Legumes such as lentils, chickpeas, and black beans: Plant-based powerhouses, rich in protein and fiber.
- Tofu and tempeh: Soy-based options offering complete protein and often used in vegetarian and vegan diets.
- Eggs: A highly bioavailable protein source, providing essential nutrients.
- Low-fat dairy: Options like Greek yogurt or cottage cheese can be good protein additions in moderation.
Healthy Fats: The Power of Omega-3 Fatty Acids for Anti-Inflammation
Not all fats are created equal. While some fats harm the liver, healthy fats, particularly those rich in omega-3 fatty acids, are incredibly beneficial due to their potent anti-inflammatory properties. These fats can help reduce liver inflammation and fat accumulation. Think of sources like fatty fish (salmon, mackerel, sardines), flaxseeds, chia seeds, and walnuts. Incorporating healthy monounsaturated fats from avocado and olive oil in moderation can also support overall metabolic health and reduce oxidative stress on the liver.
Vibrant Fruits and Vegetables: Antioxidant Powerhouses for Your Liver
“Eat the rainbow” isn’t just a catchy phrase; it’s a powerful strategy for liver health. Fruits and vegetables are packed with antioxidants, vitamins, and minerals that protect liver cells from damage caused by free radicals. Berries, citrus fruits, leafy greens (spinach, kale), broccoli, cauliflower, carrots, and beets are particularly rich in compounds that support detoxification pathways and reduce inflammation. Aim for a wide variety to ensure you’re getting a broad spectrum of protective nutrients. These colorful additions are crucial for an anti-inflammatory foods liver strategy.
Beverages for Liver Support: Hydration and Beneficial Herbal Infusions
Staying well-hydrated is fundamental for all bodily functions, including those of the liver. Water is always the best choice. Beyond plain water, certain beverages can offer additional liver benefits. Green tea, for example, is rich in catechins, powerful antioxidants shown to improve liver enzyme levels and reduce liver fat in some studies. Coffee, in moderation, has also been linked to a reduced risk of liver disease progression. Herbal infusions like dandelion tea or milk thistle tea are often touted for liver support, but it’s essential to consult your doctor before using them, especially if you’re on medication.
Foods and Habits to Limit or Avoid for Optimal Liver Function
Just as important as knowing what to eat is understanding what to limit or eliminate. These dietary culprits often exacerbate hepatic steatosis by increasing fat storage, promoting inflammation, and contributing to insulin resistance. Making these adjustments is not about punishment, but about giving your liver a much-needed break.

Minimizing Added Sugars and Refined Carbohydrates: Tackling Insulin Resistance
This is arguably the most critical step. Added sugars (found in sodas, fruit juices, candy, pastries, sweetened yogurts) and refined carbohydrates (white bread, white rice, pasta made from refined flour) are rapidly broken down into glucose, spiking blood sugar and demanding high insulin release. This constant flood of glucose is directly converted into fat in the liver, fueling NAFLD progression. Reducing these is central to managing insulin resistance fatty liver and reversing fat buildup. Read labels carefully – sugar hides under many names, like high-fructose corn syrup, dextrose, and maltose.
Reducing Unhealthy Fats: Saturated, Trans, and Highly Processed Oils
While healthy fats are beneficial, unhealthy fats actively harm your liver.
- Saturated fats (found in fatty meats, butter, full-fat dairy, some tropical oils like coconut and palm oil) can increase liver fat and inflammation.
- Trans fats (often in fried foods, baked goods, and some margarines) are particularly detrimental and should be avoided entirely.
- Highly processed vegetable oils (like corn, soybean, and sunflower oil when consumed in excess and especially if deep-fried) contain omega-6 fatty acids that, in imbalance with omega-3s, can promote inflammation. Choose healthier cooking oils like olive oil or avocado oil in moderation.
The Impact of Processed Foods and Excessive Sodium on Liver Wellness
Processed foods are typically a triple threat: high in unhealthy fats, added sugars, and excessive sodium. Think packaged snacks, fast food, frozen dinners, and cured meats. These foods offer little nutritional value and burden the liver with artificial ingredients and preservatives.
Excessive sodium intake, common in processed foods, can contribute to fluid retention and high blood pressure, indirectly stressing the liver and potentially worsening liver scarring. Aim for fresh, whole foods that you prepare yourself to control these harmful ingredients.
Alcohol Consumption: A Critical Consideration for Non-Alcoholic Fatty Liver Disease
Despite the “non-alcoholic” in NAFLD, alcohol consumption can still be problematic. Even moderate amounts of alcohol can place additional strain on a liver already compromised by fat buildup, potentially accelerating inflammation and damage. For individuals with NAFLD, particularly those with more advanced stages or those at risk of progression, healthcare professionals often recommend complete abstinence from alcohol. It’s a vital step to minimize further liver injury and support healing.
Crafting Your Liver-Friendly Plate: Practical Meal Planning Strategies
Transitioning to a diet for fatty liver is more manageable with a clear plan. It’s about building sustainable habits, not just short-term fixes. By focusing on whole foods and smart preparation, you can create delicious meals that actively support your liver’s recovery.

Building Balanced Meals: Portion Control and Nutrient Distribution
The key to a liver-friendly plate lies in portion control and a balanced distribution of macronutrients. Aim for meals that are:
- Half non-starchy vegetables: Broccoli, spinach, peppers, green beans.
- A quarter lean protein: Fish, chicken, tofu, lentils.
- A quarter complex carbohydrates: Brown rice, quinoa, sweet potato.
A small amount of healthy fats (e.g., olive oil dressing, avocado) should also be incorporated. This approach ensures you’re getting ample fiber, antioxidants, and protein without overconsuming calories or rapidly digestible carbohydrates that can turn into liver fat.
Snacking Smart: Healthy Choices Between Main Meals
Snacking is often where hidden sugars and unhealthy fats creep into our diets. For a best diet for NAFLD, intelligent snacking is crucial. Opt for options that provide sustained energy and satiety without spiking blood sugar.
- A handful of unsalted almonds or walnuts.
- Greek yogurt with a few berries.
- Apple slices with a tablespoon of natural peanut butter.
- Carrot sticks or cucumber slices with hummus.
These choices curb hunger, prevent overeating at main meals, and provide beneficial nutrients.
Sample Liver-Healthy Meal Ideas for Breakfast, Lunch, and Dinner
Here’s a practical table with meal suggestions to kickstart your NAFLD diet plan:
| Meal Type | Example Dish | Key Liver-Friendly Ingredients |
|---|---|---|
| :——– | :———————————————— | :————————————————————- |
| Breakfast | Oatmeal with Berries and Chia Seeds | Fiber (oats, berries), Antioxidants (berries), Omega-3s (chia) |
| Lunch | Lentil Soup with Whole-Wheat Bread | Lean Protein (lentils), Fiber (lentils, bread), Vegetables |
| Dinner | Baked Salmon with Roasted Broccoli and Quinoa | Omega-3s (salmon), Antioxidants (broccoli), Complex Carbs (quinoa) |
| Snack | Apple Slices with Almond Butter | Fiber (apple), Healthy Fats & Protein (almond butter) |
Navigating Iranian Cuisine with a Liver-Healthy Twist: Smart Substitutions
Iranian cuisine is rich, flavorful, and often incorporates rice, legumes, and fresh herbs. With a few smart substitutions, you can enjoy traditional dishes while supporting your liver:
- Rice: Swap white rice (chelo) for brown rice or whole-grain basmati in dishes like Adas Polo or Sabzi Polo.
- Oil: Reduce the amount of oil used in stews (Khoresh) and pilafs. Use healthier oils like olive oil in moderation.
- Sweets: Minimize sugary desserts (Halva, Sholeh Zard) or opt for naturally sweet fruits.
- Meat: Choose leaner cuts of meat for kebabs or stews, and increase the vegetable and legume content. For Ghormeh Sabzi, focus on plenty of fresh herbs and beans with smaller portions of lean beef or lamb. Consider plant-based versions with lentils.
- Dough: While refreshing, reduce the sugar content in Dough (yogurt drink) or opt for plain yogurt.
These small changes can make a big difference in making Iranian cuisine more liver-friendly.
Understanding Food Labels: Making Informed Dietary Choices
Becoming a savvy label reader is an essential skill. Look beyond front-of-package claims and focus on the Nutrition Facts panel and ingredient list.
- Added Sugars: Prioritize foods with zero or very low added sugars.
- Fiber: Aim for foods high in dietary fiber.
- Fats: Check for saturated and trans fats, aiming to minimize them.
- Sodium: Choose low-sodium options.
- Ingredients List: Opt for foods with short ingredient lists, featuring whole, recognizable ingredients. A long list with unpronounceable chemicals often indicates a highly processed item.
Beyond Diet: Lifestyle Adjustments for Comprehensive Liver Health
While diet is paramount, true liver health nutrition encompasses a broader holistic approach. Our lifestyle choices profoundly impact our liver’s ability to heal and function optimally. Integrating these habits amplifies the positive effects of your dietary changes.

The Indispensable Role of Regular Physical Activity in NAFLD Management
Exercise isn’t just for weight loss; it directly improves liver health. Regular physical activity, even moderate intensity like brisk walking, helps reduce insulin resistance, decreases liver fat, and improves liver enzyme levels, independent of significant weight loss. Aim for at least 150 minutes of moderate-intensity aerobic activity per week, along with two days of strength training. Find an activity you enjoy, whether it’s cycling, swimming, dancing, or even gardening, to make it sustainable.
Maintaining a Healthy Weight: A Cornerstone of Liver Improvement
For many with NAFLD, carrying excess weight is a significant contributor to their condition. Achieving and maintaining a healthy weight is one of the most effective strategies for reversing liver fat and preventing progression. Even a modest weight loss of 5-10% of your body weight can lead to significant reductions in liver fat and inflammation. This is why the dietary changes and increased physical activity discussed earlier are so powerful – they work synergistically to support healthy weight management.
Stress Management and Adequate Sleep: Indirect but Important Factors for Hepatic Well-being
It might seem indirect, but chronic stress can affect metabolic health and inflammation, potentially impacting the liver. Finding healthy ways to manage stress – through mindfulness, meditation, yoga, spending time in nature, or hobbies – can support overall well-being. Similarly, adequate sleep (7-9 hours per night for most adults) is crucial for hormonal balance and metabolic regulation. Poor sleep can contribute to insulin resistance and weight gain, making liver healing more challenging. Prioritizing rest is a silent but powerful ally in your journey to a healthier liver.
Hydration: The Simple Yet Powerful Practice for Overall Health
We touched on beneficial beverages earlier, but it bears repeating: sufficient hydration with plain water is fundamental. Water plays a crucial role in detoxification processes, helping the kidneys and liver flush out waste products. It also aids in digestion and nutrient transport. Make water your primary beverage, aiming for at least 8 glasses a day, and more if you’re physically active or in a hot climate.
Empowering Your Journey to a Healthier Liver
Taking control of your liver health is a marathon, not a sprint. It requires commitment, patience, and a willingness to learn and adapt. But with the right knowledge and a proactive mindset, you have the power to make significant improvements and live a fuller, healthier life.

Monitoring Progress and Collaborating with Healthcare Professionals
Regular follow-ups with your doctor are crucial for monitoring your progress. This typically involves blood tests to check liver enzyme levels, sometimes imaging tests like ultrasound, or even more advanced scans to assess liver fat and fibrosis. Your healthcare team, including a doctor, dietitian, or hepatologist, can provide personalized guidance, adjust your plan as needed, and address any concerns. Don’t hesitate to ask questions; they are your partners in this journey.
Dispelling Common Myths and Misconceptions About Fatty Liver Diets
There’s a lot of misinformation out there. It’s important to stick to evidence-based advice.
- Myth: “Juice cleanses will detox your liver.” Reality: Your liver is a powerful detox organ; it doesn’t need special cleanses. Focus on a balanced, whole-food diet.
- Myth: “You can eat anything as long as you take a supplement.” Reality: While some supplements might support liver health, they are never a substitute for dietary and lifestyle changes. Always consult your doctor before starting any supplement.
- Myth: “A fatty liver diet means no flavor.” Reality: With fresh herbs, spices, and creative cooking, a liver-friendly diet can be incredibly delicious and satisfying.
Cultivating Sustainable Habits for Long-Term Liver Wellness
The goal is not just to fix your liver today but to foster long-term wellness. Focus on small, consistent changes that you can maintain indefinitely. Celebrate your successes, learn from setbacks, and be kind to yourself. Building sustainable habits around healthy eating, regular activity, and self-care will not only benefit your liver but will also enhance your overall vitality and quality of life for years to come. Your liver will thank you.
Conclusion & Takeaways
Navigating a diagnosis of fatty liver disease can feel overwhelming, but by taking proactive steps with your diet and lifestyle, you hold immense power to improve your health. Remember, the core principles are simple: prioritize whole, unprocessed foods, embrace fiber-rich grains, lean proteins, and healthy fats, and consciously limit added sugars, refined carbohydrates, and unhealthy fats. Couple these dietary changes with regular physical activity, adequate sleep, and stress management, and you’re building a formidable foundation for liver health nutrition. This isn’t just about managing a condition; it’s about embracing a lifestyle that empowers your liver to heal, thrive, and serve you well for a lifetime. Start today, one healthy choice at a time, and reclaim your wellness.
FAQ
What foods should I absolutely avoid if I have fatty liver?
To protect your liver, absolutely minimize or avoid sugary drinks (sodas, fruit juices), foods high in added sugars (candies, pastries), trans fats (fried foods, many processed snacks), and excessive refined carbohydrates (white bread, white rice). Limiting saturated fats from fatty meats and full-fat dairy is also crucial, and for NAFLD, alcohol consumption should be critically re-evaluated with your doctor, often leading to abstinence.
Can changing my diet really reverse fatty liver disease?
Yes, for many individuals, significant dietary and lifestyle changes can lead to the reversal of non-alcoholic fatty liver disease (NAFLD). Studies show that even a modest weight loss (5-10% of body weight) achieved through diet and exercise can substantially reduce liver fat, improve inflammation, and normalize liver enzyme levels. Consistency and commitment to these changes are key to successful management and potential reversal.
Are there specific superfoods that help improve fatty liver?
While no single “superfood” is a magical cure, certain foods are particularly beneficial for liver health due to their nutrient profile. These include foods rich in omega-3 fatty acids (like salmon, flaxseeds), fiber (oats, legumes, whole grains), and antioxidants (berries, green leafy vegetables, green tea). These foods help reduce inflammation, improve insulin sensitivity, and support overall liver function, making them excellent choices within a balanced liver-healthy diet.














