It’s a familiar story: years of restless nights, persistent daytime fatigue, and the disruptive sound of snoring. For many, this points to Obstructive Sleep Apnea (OSA), a condition affecting millions globally, often exacerbated by metabolic challenges. Just last year, my own uncle, after battling type 2 diabetes and obesity, received an OSA diagnosis. His journey with a new class of medications, GLP-1 receptor agonists, has since opened a fascinating door to improved sleep and overall well-being. This emerging connection between metabolic health and respiratory function is changing the landscape of OSA management, offering a hopeful new frontier for those seeking relief. Join us as we explore the science behind this promising link.
The Emerging Connection: GLP-1 Agonists and Sleep Apnea
The conversation around GLP-1 receptor agonists has largely centered on their revolutionary impact in managing type 2 diabetes and facilitating significant weight loss. However, a compelling narrative is unfolding, suggesting these medications may offer far-reaching benefits, specifically for individuals grappling with Obstructive Sleep Apnea (OSA). This isn’t just about weight; it’s about a deeper, systemic influence on metabolic health that could reshape how we approach sleep-disordered breathing. This section delves into the foundational understanding of this intriguing, multifaceted relationship.

A New Frontier in Sleep Health Management
For too long, Obstructive Sleep Apnea management has relied primarily on mechanical solutions like Continuous Positive Airway Pressure (CPAP) or surgical interventions. While effective, these don’t always address the underlying metabolic dysfunctions often intertwined with OSA. The advent of GLP-1 receptor agonists introduces a biological pathway, hinting at a potential to not just alleviate symptoms, but also to tackle core contributors to the condition. This represents a significant shift, expanding our therapeutic toolkit beyond traditional methods.
Bridging Metabolic Health and Respiratory Well-being
The human body is an intricate network, where metabolic health profoundly influences nearly every system, including respiratory function. GLP-1 receptor agonists work by mimicking a natural hormone that helps regulate blood sugar, slows gastric emptying, and reduces appetite. These actions, particularly the significant weight loss they can induce, are now being investigated for their beneficial ripple effect on the physical and physiological factors contributing to OSA. The link suggests a holistic approach that simultaneously targets metabolic and respiratory health.
Why the Link Between GLP-1 and OSA Matters
The prevalence of OSA is significantly higher in individuals with obesity and metabolic syndrome. By addressing these foundational issues, GLP-1 medications offer a promising avenue to improve OSA outcomes, potentially reducing the severity of apneas and hypopneas. This connection is vital because it moves beyond mere symptom management toward addressing the underlying comorbidities that often fuel sleep apnea.
Defining GLP-1 Receptor Agonists and Obstructive Sleep Apnea
To understand their interplay, it’s crucial to define these key players. GLP-1 receptor agonists are a class of medications that activate the GLP-1 receptor, leading to glucose-dependent insulin secretion, slowed gastric emptying, and appetite suppression. Meanwhile, Obstructive Sleep Apnea (OSA) is a common sleep disorder characterized by repeated episodes of complete or partial upper airway obstruction during sleep, leading to reduced or absent breathing. Understanding these definitions is the first step toward appreciating their potential synergy.
Understanding Obstructive Sleep Apnea (OSA): More Than Just Snoring
Many people mistakenly believe snoring is just an annoying nightly habit. However, for millions, it’s a critical red flag for Obstructive Sleep Apnea (OSA), a serious condition characterized by repeated pauses in breathing during sleep. This disorder doesn’t just disrupt sleep; it significantly impacts overall health, often going undiagnosed for years. Understanding the mechanics, risk factors, and profound health consequences of OSA is crucial for appreciating new therapeutic avenues like GLP-1 medications.
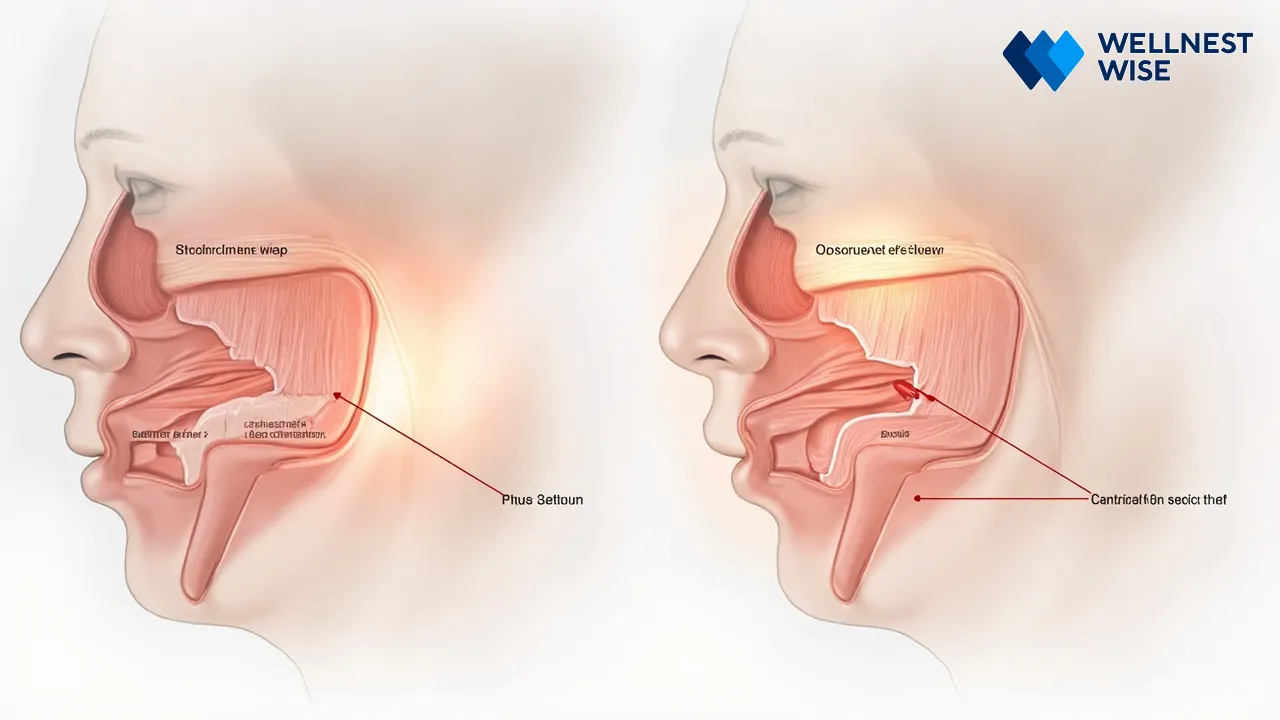
The Pathophysiology of Obstructive Sleep Apnea
At its core, Obstructive Sleep Apnea occurs when the muscles in the back of your throat relax too much to allow normal breathing. This causes the soft palate, tonsils, and tongue to collapse, partially or completely blocking the airway. When this happens, your brain briefly wakes you up to reopen the airway, often without your conscious awareness, leading to fragmented sleep and reduced oxygen levels. This cycle can repeat hundreds of times a night, preventing deep, restorative sleep.
What Happens During an Apnea Event
During an apnea event, breathing stops for at least 10 seconds. Your body responds with a surge of adrenaline, elevating heart rate and blood pressure as it struggles to resume breathing. This repeated stress on the cardiovascular system, combined with intermittent oxygen deprivation (hypoxia), sets the stage for a host of health complications. The “fight or flight” response triggered nightly is anything but restful.
Common Risk Factors and Associated Health Complications
Several factors increase the likelihood of developing OSA. Many of these are intricately linked to metabolic health, making GLP-1 receptor agonists a particularly interesting area of investigation.
- Obesity and Body Mass Index (BMI): A primary driver of airway collapse, often associated with insulin resistance and increased fat deposits around the neck and throat, narrowing the airway.
- Anatomical Structures: Enlarged tonsils, adenoids, a soft palate, or a large tongue can contribute to upper airway obstruction.
- Age and Gender: Increased risk with advancing age, often more prevalent in men pre-menopause due to hormonal differences.
- Lifestyle Factors: Alcohol consumption, smoking, and sedative use can relax throat muscles, worsening sleep-disordered breathing.
- Underlying Health Conditions: Hypothyroidism, acromegaly, and metabolic syndrome significantly impact respiratory control and tissue swelling.
The Impact of Untreated OSA on Overall Health and Quality of Life
The consequences of untreated OSA extend far beyond daytime sleepiness. It’s a silent threat that gradually erodes health, impacting nearly every aspect of life. According to the National Heart, Lung, and Blood Institute (NHLBI), the long-term effects are severe, reinforcing the urgent need for effective management strategies.
Long-term Health Consequences: Cardiovascular and Metabolic Risks
Untreated OSA significantly increases the risk for serious health issues. The repeated drops in blood oxygen and surges in stress hormones contribute to:
- High blood pressure (hypertension)
- Heart attack and stroke
- Irregular heartbeats (arrhythmias)
- Type 2 diabetes and worsening insulin resistance
- Metabolic syndrome
Daily Challenges: Fatigue, Concentration, and Mood Impairments
Beyond the physical risks, the daily toll of untreated OSA is immense. Chronic sleep deprivation leads to:
- Excessive daytime fatigue and drowsiness, increasing accident risk
- Difficulty concentrating, memory problems, and reduced productivity
- Irritability, mood swings, and an increased risk of depression
- Impaired quality of life and reduced overall well-being
The Role of GLP-1 Receptor Agonists: Beyond Diabetes and Weight Management
Initially celebrated for their groundbreaking effects on blood sugar control and weight loss, GLP-1 receptor agonists are now revealing a broader spectrum of therapeutic potential. These medications, once primarily known within endocrinology circles, are gaining recognition for their systemic benefits, hinting at an exciting future in managing conditions like Obstructive Sleep Apnea (OSA). This section explores what these medications are, how they work, and their established uses, setting the stage for their emerging role in sleep health.

What Are GLP-1 Receptor Agonists?
GLP-1 receptor agonists are a class of drugs designed to mimic the action of glucagon-like peptide-1, a natural hormone produced in the gut. This hormone plays a crucial role in regulating appetite, glucose metabolism, and gastric emptying. By activating GLP-1 receptors, these medications essentially trick your body into thinking it has more of this natural hormone, leading to a cascade of beneficial effects.
How These Medications Function at a Cellular Level
At a cellular level, GLP-1 receptor agonists bind to GLP-1 receptors in various tissues, including the pancreas, brain, and gut. In the pancreas, they stimulate insulin secretion in a glucose-dependent manner (meaning it only works when blood sugar is high), and suppress glucagon release. In the brain, they influence satiety centers, reducing hunger. This multi-pronged action contributes to their profound effects on metabolic health.
Primary Therapeutic Uses: Diabetes and Weight Management
The primary, FDA-approved indications for GLP-1 receptor agonists are the treatment of type 2 diabetes and chronic weight management. For individuals with type 2 diabetes, these medications help lower HbA1c, improve glycemic control, and can offer cardiovascular benefits. For those struggling with obesity, they provide a powerful tool for achieving significant and sustainable weight loss when combined with diet and exercise.
The Mechanism Behind Significant Weight Loss with GLP-1 Medications
The weight loss observed with GLP-1 medications is primarily driven by their effect on appetite suppression and satiety. By slowing gastric emptying, they help you feel fuller for longer. Furthermore, their action on brain pathways reduces food cravings and overall calorie intake. This leads to a caloric deficit that, over time, results in substantial weight reduction, a key factor in improving conditions like OSA.
Understanding Key GLP-1 Medications: Ozempic, Wegovy, and More
This class of medications includes several notable drugs, each with specific indications and dosing schedules. While all work by activating GLP-1 receptors, there are differences in their chemical structure, duration of action, and approved uses.
| Medication Name (Generic) | Brand Names | Primary FDA-Approved Indications | Typical Dosage Frequency |
|---|---|---|---|
| :———————— | :—————————————– | :————————————————— | :———————– |
| Semaglutide | Ozempic (diabetes), Wegovy (weight loss), Rybelsus (oral diabetes) | Type 2 Diabetes, Chronic Weight Management | Weekly |
| Liraglutide | Victoza (diabetes), Saxenda (weight loss) | Type 2 Diabetes, Chronic Weight Management | Daily |
| Dulaglutide | Trulicity | Type 2 Diabetes, Cardiovascular Risk Reduction | Weekly |
| Exenatide | Byetta, Bydureon BCise | Type 2 Diabetes | Twice daily / Weekly |
Mechanisms of Action: How GLP-1 May Improve Sleep Apnea Symptoms
The potential of GLP-1 receptor agonists to mitigate Obstructive Sleep Apnea (OSA) symptoms is an exciting area of research, extending beyond their established roles in diabetes and weight management. This improvement isn’t merely coincidental; it’s thought to stem from a fascinating interplay of both indirect and potentially direct physiological effects. Understanding these mechanisms helps us grasp why these medications are emerging as a promising adjunctive therapy for better sleep and respiratory health.
Indirect Benefits: The Critical Role of Weight Loss
The most well-established and significant way GLP-1 medications are believed to improve OSA is through substantial weight loss. Obesity is, after all, the single greatest risk factor for developing and worsening sleep apnea. By helping individuals shed excess pounds, these medications directly address the primary mechanical cause of airway obstruction.
Reducing Upper Airway Obstruction Through Body Mass Index (BMI) Reduction
When an individual loses a significant amount of weight, particularly around the neck and pharynx, the fat pads that contribute to airway narrowing are reduced. This leads to a more open and stable upper airway during sleep. A reduction in body mass index (BMI) often translates directly to a decrease in the frequency and severity of apnea-hypopnea index (AHI) events, which is the key measure of OSA severity. For my uncle, who was struggling with moderate OSA, the noticeable weight loss achieved with his GLP-1 medication was accompanied by a clear reduction in his snoring and a subjective improvement in his sleep quality, even before his formal re-evaluation.
Direct Physiological Effects on Sleep Apnea Severity
Beyond weight loss, emerging evidence suggests that GLP-1 receptor agonists might exert more direct physiological benefits that could influence OSA severity. These effects delve into the intricate relationship between metabolic health, inflammation, and respiratory control.
Modulating Systemic Inflammation and Oxidative Stress Pathways
Obstructive Sleep Apnea itself is known to induce systemic inflammation and oxidative stress due to intermittent hypoxia. These inflammatory processes can contribute to tissue swelling in the upper airway, further exacerbating obstruction. GLP-1 receptor agonists have demonstrated anti-inflammatory properties, potentially reducing the inflammation that contributes to airway instability. By dampening this inflammatory cascade, they could offer a direct protective effect on the airway.
Influencing Metabolic Health and Insulin Resistance
OSA often coexists with insulin resistance and metabolic syndrome, creating a vicious cycle where each condition worsens the other. GLP-1 medications are highly effective at improving insulin sensitivity and metabolic parameters. Better metabolic control can lead to a healthier cellular environment, which may, in turn, reduce the propensity for fluid retention and tissue swelling in the upper airway, providing a direct benefit to breathing during sleep.
Potential Effects on Respiratory Control and Upper Airway Muscle Tone
This is perhaps the most intriguing, yet least understood, potential direct mechanism. Some preclinical research indicates that GLP-1 receptors are present in areas of the brain involved in respiratory control. It’s hypothesized that GLP-1 agonists might directly modulate neural pathways that govern breathing and the tone of upper airway muscles, making them less prone to collapse during sleep. While this area requires further robust clinical investigation, it suggests a profound impact beyond just weight.
Current Research and Clinical Perspectives on GLP-1 for OSA
The intersection of GLP-1 receptor agonists and Obstructive Sleep Apnea (OSA) represents a dynamic and rapidly evolving field of scientific inquiry. While their primary applications in diabetes and weight management are well-established, a growing body of research is exploring their potential in sleep medicine. This section provides an overview of what the science is saying, the nuances in understanding their benefits, and the expert outlook on their future role.

Emerging Clinical Trial Data and Observational Studies
Initial findings from both clinical trials and observational studies are quite encouraging. Researchers are seeing consistent trends where patients receiving GLP-1 receptor agonists for diabetes or obesity experience improvements in their sleep apnea symptoms. Many studies report reductions in the apnea-hypopnea index (AHI), often correlating with the degree of weight loss achieved.
What the Science Says So Far About GLP-1 Benefits on Sleep Apnea Severity
A significant portion of the observed benefits points to the profound impact of weight reduction. For instance, data indicates that a 10% or greater weight loss can lead to a meaningful reduction in AHI. However, some preliminary findings suggest that improvements might occur even independent of, or disproportionately to, the weight lost, hinting at the direct physiological mechanisms we discussed earlier. While direct, large-scale, randomized controlled trials specifically on GLP-1s for OSA are still relatively nascent, the existing evidence strongly supports a positive association.
Expert Insight: “While GLP-1 receptor agonists are not yet FDA-approved specifically for sleep apnea, the data we’re seeing, particularly in patients with obesity, is compelling. It reinforces the critical link between metabolic health and respiratory well-being. We’re moving towards a more integrated approach to these complex conditions.” – Leading endocrinologist specializing in metabolic health.
Distinguishing Between Direct and Indirect Improvements in AHI
A key challenge in the research is precisely dissecting whether the improvement in AHI is solely due to weight loss (indirect effect) or if there are direct effects on factors like inflammation, insulin resistance, or respiratory control mechanisms. While weight loss is undeniably a major contributor, some studies are attempting to control for weight loss to isolate any direct effects, though robust conclusions still require more extensive research. The general consensus points to a synergistic effect, where both mechanisms likely play a role.
Expert Opinions and Future Directions in Novel Therapies for OSA
Experts in both endocrinology and sleep medicine view GLP-1 receptor agonists as a promising addition to the therapeutic landscape for OSA, especially for patients with co-existing obesity and metabolic disorders. The focus is shifting towards personalized medicine, where such medications could be tailored to individuals who stand to benefit the most.
The Role of GLP-1 Receptor Agonists as Adjuvant Therapy to CPAP
It’s important to clarify that GLP-1 receptor agonists are not currently seen as a standalone cure or replacement for established OSA treatments like CPAP therapy. Instead, they are being considered as an adjunct therapy. This means they could be used in addition to CPAP, potentially improving CPAP adherence (due to better energy levels), reducing CPAP pressure requirements, or even making CPAP unnecessary for some individuals who achieve significant improvements. My uncle’s experience, where his endocrinologist suggested a GLP-1 alongside his prescribed CPAP, exemplifies this combined approach, improving his overall metabolic health and reducing the severity of his OSA symptoms.
Limitations of Current Research and Knowledge Gaps
Despite the optimism, it’s crucial to acknowledge the limitations. Most studies to date have been relatively small or observational. There is a need for larger, double-blind, placebo-controlled trials specifically designed to evaluate GLP-1 receptor agonists as a treatment for OSA, independent of or in conjunction with weight loss. Further research is also needed to fully elucidate the direct mechanisms of action on respiratory physiology and to understand the long-term effects. This will provide the robust evidence required for potential future FDA approvals for this specific indication.
Navigating Treatment: Important Considerations and Future Outlook
The prospect of GLP-1 receptor agonists offering benefits for Obstructive Sleep Apnea (OSA) is undeniably exciting, particularly for those whose condition is intertwined with obesity or metabolic issues. However, navigating this emerging therapeutic avenue requires careful consideration, informed decision-making, and, most importantly, personalized medical guidance. This section outlines when to consider these medications, their safety profile, and the crucial role of your healthcare professional in integrating them into a comprehensive OSA treatment plan.

When to Consider GLP-1 Agonists for Sleep Apnea
Considering GLP-1 receptor agonists for OSA is not a universal recommendation but rather a discussion point for specific patient profiles. They are primarily indicated for individuals with type 2 diabetes or those with obesity (BMI ≥30 kg/m² or ≥27 kg/m² with at least one weight-related comorbidity). The potential for OSA improvement adds another layer of benefit for these individuals.
Eligibility Criteria and Co-occurring Metabolic Conditions
If you have been diagnosed with Obstructive Sleep Apnea and also have co-occurring metabolic conditions like type 2 diabetes, insulin resistance, or obesity, then discussing GLP-1 medications with your doctor becomes highly relevant. These medications address the underlying metabolic dysfunctions that often contribute to OSA, making them a synergistic choice for those with these specific comorbidities.
Understanding Potential Side Effects and Safety Profiles
Like all medications, GLP-1 receptor agonists come with potential side effects. The most common are gastrointestinal, including nausea, vomiting, diarrhea, and constipation, which usually lessen over time. More serious but rare side effects include pancreatitis, gallbladder issues, and thyroid C-cell tumors (seen in rodent studies, but human relevance is uncertain). A thorough discussion with your doctor about your medical history and potential risks is essential before starting any treatment.
The Importance of a Comprehensive Treatment Plan for OSA
It is crucial to remember that GLP-1 medications are not a standalone “cure” for OSA. Effective obstructive sleep apnea management typically involves a multi-faceted approach. This often includes lifestyle modifications (diet, exercise), and for many, adherence to CPAP therapy. The emerging role of GLP-1s is as an adjunctive therapy, complementing existing treatments rather than replacing them.
Integrating GLP-1 Medications with Existing Therapies like CPAP
For individuals already using CPAP, incorporating a GLP-1 receptor agonist could potentially lead to reduced CPAP pressure requirements, improved comfort, and better overall adherence due to enhanced energy and metabolic health. It’s about optimizing all possible avenues to achieve the best respiratory and overall health outcomes. This comprehensive strategy, as observed in my uncle’s case, can significantly improve quality of life by tackling the problem from multiple angles.
Consulting Your Healthcare Professional: A Personalized Approach
Given the complexity of Obstructive Sleep Apnea and the systemic effects of GLP-1 receptor agonists, expert medical guidance is non-negotiable. Only a qualified healthcare provider can assess your individual health profile, diagnose your specific conditions, and determine if GLP-1 medications are appropriate for you.
Why Expert Medical Guidance is Essential for GLP-1 Use in Sleep Apnea
Your doctor, ideally a sleep specialist or endocrinologist, will evaluate your medical history, current medications, and the severity of your OSA and metabolic conditions. They can weigh the potential benefits against any risks, monitor your progress, and adjust your treatment plan as needed. Self-medication or making treatment decisions without professional oversight can be dangerous and is strongly discouraged.
The Promising Future of GLP-1 in Obstructive Sleep Apnea Management
The research linking GLP-1 receptor agonists to improved Obstructive Sleep Apnea outcomes is still unfolding, but the early indications are profoundly promising. As our understanding of the intricate connections between metabolic health, inflammation, and respiratory control deepens, these medications may play an increasingly vital role in comprehensive OSA management. For many, this could mean not just better sleep, but a pathway to significantly improved overall health and a higher quality of life.
Conclusion & Takeaways
The journey to understand and treat Obstructive Sleep Apnea (OSA) is continuously evolving, and the emergence of GLP-1 receptor agonists marks a significant and hopeful new chapter. While primarily known for their powerful effects on type 2 diabetes and weight management, a growing body of evidence suggests these medications can profoundly impact OSA severity, particularly for individuals with co-existing obesity and metabolic challenges. The benefits appear to stem from both the direct mechanical advantage of weight loss—reducing physical obstruction in the airway—and potentially direct physiological effects like modulating systemic inflammation, improving insulin resistance, and even influencing respiratory control centers.
It’s crucial to understand that GLP-1 medications are not yet a standalone, FDA-approved treatment for OSA, but rather a promising adjunctive therapy. They work best within a comprehensive treatment strategy, often alongside established methods like CPAP therapy and targeted lifestyle changes. For many, including individuals like my uncle, this integrated approach offers a pathway to not just clearer airways but improved overall metabolic health, renewed energy, and a significantly enhanced quality of life. As research continues to unravel the full spectrum of their effects, the future of obstructive sleep apnea management appears to be moving towards more personalized, metabolically-focused interventions. If you’re struggling with OSA, especially with underlying metabolic conditions, consult your healthcare provider to discuss whether GLP-1 receptor agonists could be a beneficial addition to your personalized treatment plan.
FAQ
Practical, scientific Q&A
Q1: Can GLP-1 medications directly improve sleep apnea, or is it solely due to weight loss?
A1: While significant weight loss (an indirect effect) is a major contributor to GLP-1 receptor agonists improving Obstructive Sleep Apnea (OSA), emerging research suggests there may also be direct physiological effects. These include modulating systemic inflammation, improving insulin resistance, and potentially influencing neural respiratory control and upper airway muscle tone. The current understanding points to a combination of both indirect and direct mechanisms working synergistically.
Q2: What are the risks and benefits of using GLP-1 agonists for sleep apnea?
A2: The primary benefit for sleep apnea patients is the potential for reduced apnea-hypopnea index (AHI) and improved sleep quality, especially in individuals with obesity and metabolic syndrome. Benefits also include weight loss and improved glycemic control. Risks include common gastrointestinal side effects (nausea, vomiting, diarrhea) and rare but serious adverse events such as pancreatitis or gallbladder issues. A thorough discussion with a healthcare professional is essential to weigh individual risks and benefits.
Q3: Are there clinical trials or studies currently investigating GLP-1s as a sleep apnea treatment?
A3: Yes, there are ongoing clinical trials and observational studies investigating the efficacy of GLP-1 receptor agonists in improving Obstructive Sleep Apnea symptoms and severity. While initial findings are promising, demonstrating reductions in AHI, particularly in conjunction with weight loss, larger-scale, randomized controlled trials are still needed to provide definitive evidence for GLP-1s as a direct, FDA-approved treatment specifically for OSA. Most current benefits are noted in patients prescribed GLP-1s for diabetes or weight management.














